The Future is Now: How to Monitor Blood Glucose Without Pricking Finger in 2025 and Beyond

For millions managing diabetes, the pain and inconvenience of fingerstick blood glucose testing are daily challenges. The desire to monitor blood glucose without pricking finger represents a pivotal goal in diabetes technology. Thanks to transformative advancements in 2025, this goal is increasingly achievable with sophisticated, non-invasive glucose monitoring technologies delivering continuous, painless, accurate results.
In this article, we explore present and emerging methods revolutionizing blood glucose monitoring, focus on their principles, benefits, and challenges, and highlight how innovations like Linx CGM exemplify progress toward an easier, more comfortable diabetes life.
The Imperative for Needle-Free Blood Glucose Monitoring
Despite the critical importance of glucose monitoring, traditional fingerstick testing remains problematic due to:
-
Repeated Pain and Discomfort: Lancet-based punctures cause soreness, infection risk, and skin damage.
-
Reduced Testing Frequency: Fear or hassle leads to infrequent measurements and poorer glycemic control.
-
Interruption of Daily Routine: Necessitating preparation, equipment, and frequent breaks disrupts activities.
The ability to monitor blood glucose without pricking finger promises to eliminate these barriers, fostering better patient compliance, safety, and overall well-being.
Leading Technologies in Needle-Free Glucose Monitoring
Photoplethysmography (PPG) and Optical Sensing
PPG is an optical monitoring method using light sensors to detect blood volume changes correlating with glucose fluctuations. When combined with AI algorithms, PPG sensors in wearables can capture glucose-correlated changes in tissue optical properties non-invasively, enabling continuous and real-time glucose readings without any skin penetration.
Raman Spectroscopy
This technique measures molecular vibrations by analyzing how laser light scatters when interacting with glucose molecules. Innovations like multi-spatially offset Raman spectroscopy (mμSORS) focus detection on skin’s capillary-rich layers for higher accuracy. Clinical studies have validated promising correlations between Raman-derived readings and blood glucose measurements.
Near-Infrared (NIR) and Mid-Infrared (MIR) Spectroscopy
NIR and MIR methods detect glucose by measuring how different skin layers absorb and reflect light at specific wavelengths. These signals are processed with powerful data analytics to filter noise and estimate glucose concentration non-invasively with increasing precision.
Optoacoustic Sensors and Time-Gated Mid-Infrared Optoacoustic Sensors (DIROS)
Optoacoustic techniques generate sound waves when skin absorbs pulsed light; time-gated sensors distinguish signals from capillary-rich subcutaneous layers, allowing selective glucose measurements. DIROS technology enhances specificity by focusing on blood vessel-rich dermal zones, reducing interference from upper skin layers.
Other Emerging Biosensors
Additional techniques under investigation include reverse iontophoresis (extracting glucose molecules via mild electrical currents), metabolic heat conformation, electromagnetic sensing, and smartphone-integrated biosensors. While still experimental, these methods diversify the approaches towards completely non-invasive glucose monitoring.
Advantages of Monitoring Blood Glucose Without Pricking Finger
The monitor blood glucose without pricking finger paradigm offers vast benefits:
-
Painless Experience: Eliminates usual discomfort, promoting frequent measurements.
-
Seamless Continuous Monitoring: Provides ongoing, real-time insights critical to immediate decision-making.
-
Lifestyle Compatibility: Wearables can be discreetly worn throughout various physical activities, including swimming and exercise.
-
Improved Patient Adherence: Ease and convenience encourage regular monitoring, minimizing blind spots in glucose control.
-
Remote Data Access and Caregiver Support: Enables sharing with healthcare providers and family members, particularly crucial for children or older adults.
Taken together, these transform diabetes management from a chore to an integral, unobtrusive part of daily life.
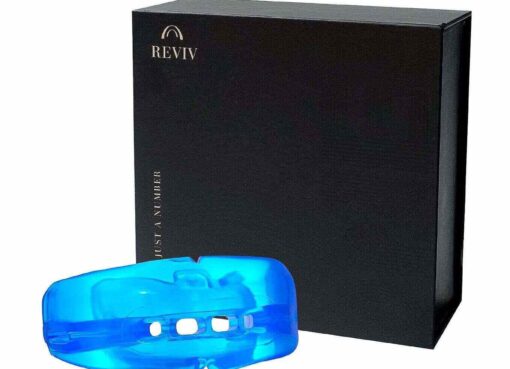
Linx CGM: Bridging Near Needle-Free Continuous Glucose Monitoring
While fully non-invasive technologies mature, Linx CGM offers a clinically advanced, minimally invasive glucose monitoring solution designed with comfort and accuracy at its core:
-
Smallest Sensor on the Market: With only 22mm in diameter and 4.2mm thickness, delivering wearability superior to traditional CGMs.
-
15-Day Sensor Life: Reduces need for frequent sensor changes, offering extended uninterrupted monitoring.
-
Waterproof IP68 Rating: Supports uninterrupted activity during swimming and exercise without compromising data integrity.
-
Optional Calibration-Free Use: Factory-set calibration removes necessity for finger prick calibrations, enhancing user convenience.
-
Smart Alerts & Remote Sharing: Enhances safety with real-time alerts and caregiver app access.
Linx CGM effectively offers near needle-free convenience with continuous, reliable glucose insights.
The Role of Artificial Intelligence in Enhancing Non-Invasive Monitoring
AI has accelerated the accuracy and usability of needle-free glucose monitoring by:
-
Advanced Signal Processing: Filtering noise and artifacts from optical and acoustic sensor data.
-
Individual Calibration: Tailoring models to account for user-specific skin types, hydration, and biological factors.
-
Predictive Analytics: Anticipating glucose excursions before occurrence to provide preemptive alerts.
-
Integration with Smart Devices: Syncing glucose data with health apps, insulin pumps, and virtual health coaches.
This synergy of AI and sensing technologies defines current and future progress in achieving seamless glucose monitoring.
Challenges and Outlook
Despite advancements, several challenges remain before universal adoption of completely non-invasive glucose monitors:
-
Reliable Hypoglycemia Detection: Ensuring high precision at low glucose ranges vital for safety.
-
Device Miniaturization and Power Efficiency: Shrinking complex optical/acoustic systems into compact, comfortable wearables.
-
Inter-User Variability: Adjusting for differences in skin composition, ambient light, temperature, and motion artifacts.
-
Regulatory Approval and Clinical Validation: Robust evidence required to satisfy health authorities worldwide.
Continuous research, clinical trials, and technology refinements are gradually overcoming these obstacles.
Future Directions: Towards Artificial Pancreas and Holistic Metabolic Health
Looking forward, monitor blood glucose without pricking finger fits into a broader future of intelligent, integrated, and holistic diabetes care:
-
Closed-Loop Automated Insulin Delivery: Blending CGM data with sophisticated insulin pumps for artificial pancreas systems.
-
Multi-Parameter Wearables: Simultaneously monitoring glucose, ketones, hydration, and other metabolic markers.
-
Telehealth and Remote Patient Monitoring: Expanding access to specialist care and personalized coaching regardless of location.
-
Personalized Medicine: AI-driven therapeutic recommendations based on comprehensive physiologic and lifestyle data.
Linx CGM stands ready to integrate and evolve within these transformative care paradigms.
Conclusion
The vision to monitor blood glucose without pricking finger is no longer distant—it is increasingly tangible in 2025 due to advancements in spectroscopy, photoplethysmography, optoacoustic sensors, and AI. These technologies promise painless, continuous, real-time glucose management, directly addressing the pain points of traditional fingerstick testing.
With Linx CGM, users gain access to one of the most compact, accurate, and easy-to-use continuous glucose monitoring solutions available today—a bridge to a needle-free future.





Leave a Comment