Flumazenil: Complete Guide to Uses, Mechanism, and Clinical Importance
Flumazenil is a medication that plays a highly specific and often life-saving role in medical practice. While many drugs treat a wide range of conditions, flumazenil is unique in that it acts almost like an antidote—its main purpose is to reverse the effects of benzodiazepines. Because of this, flumazenil is often used in emergency medicine, anesthesia, and critical care.
This article provides a comprehensive overview of flumazenil, covering its pharmacology, clinical applications, safety considerations, and the role it plays in modern healthcare.
What is Flumazenil?
Flumazenil is a benzodiazepine receptor antagonist. Unlike benzodiazepines, which enhance the effects of gamma-aminobutyric acid (GABA) in the brain and cause sedation, flumazenil blocks these effects. In simple terms, it works by “undoing” the sedative and hypnotic effects of benzodiazepines.
It is most commonly administered intravenously and has a rapid onset of action, making it useful in emergencies where quick reversal of sedation is required.
Mechanism of Action
Benzodiazepines act by binding to the GABA-A receptor complex in the brain, enhancing the inhibitory effects of GABA. This results in:
-
Sedation
-
Reduced anxiety
-
Muscle relaxation
-
Anticonvulsant effects
Flumazenil works by competitively binding to the benzodiazepine binding site on the GABA-A receptor, thereby preventing benzodiazepines from exerting their effects. This reversal can rapidly restore alertness and respiratory drive in patients who have been sedated.
Clinical Uses of Flumazenil
Flumazenil has a very specialized set of clinical indications.
Reversal of Benzodiazepine Sedation
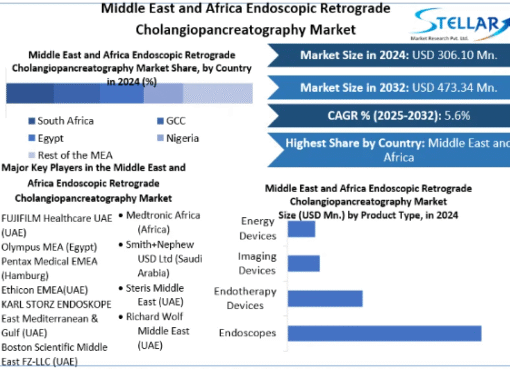
In hospital settings, benzodiazepines are often used for sedation during surgery, endoscopic procedures, or intensive care. Flumazenil can reverse these effects once the procedure is complete, helping patients regain consciousness quickly and safely.
Management of Benzodiazepine Overdose
In cases of suspected overdose, flumazenil may be used to reverse life-threatening respiratory depression or deep sedation. However, it must be used with caution, as it can precipitate withdrawal symptoms and seizures in patients with long-term benzodiazepine dependence.
Diagnostic Tool
Flumazenil can be used diagnostically to determine whether a patient’s symptoms (such as altered mental status or coma) are due to benzodiazepine use. If symptoms improve after administration, it provides a strong clue that benzodiazepines are involved.
Administration and Dosage
Flumazenil is given intravenously under medical supervision.
-
Initial dose: Usually 0.2 mg IV over 15 seconds.
-
Repeat dosing: If the patient does not respond, additional doses of 0.1 mg may be given at 1-minute intervals, up to a maximum of 1 mg.
-
Maintenance: Continuous infusion may be used if sedation recurs, but prolonged infusions increase the risk of seizures.
Because flumazenil has a short half-life (40–80 minutes), its effects may wear off before the benzodiazepine has been fully metabolized. This means that patients must be closely monitored for recurrent sedation.
Side Effects of Flumazenil
While flumazenil is generally safe when administered in a controlled setting, it does carry risks.
Common side effects include:
-
Nausea and vomiting
-
Dizziness
-
Headache
-
Sweating and flushing
-
Visual disturbances
Serious risks include:
-
Seizures – especially in patients with benzodiazepine dependence or co-ingestion of pro-convulsant drugs (e.g., tricyclic antidepressants).
-
Cardiac arrhythmias – rare but possible in at-risk patients.
-
Withdrawal symptoms – abrupt reversal can trigger anxiety, agitation, and tremors.
Because of these risks, flumazenil is never used outside of a hospital or emergency setting.
Contraindications
Flumazenil should not be used in certain scenarios:
-
Patients with chronic benzodiazepine dependence (risk of withdrawal seizures).
-
Mixed drug overdoses, especially with tricyclic antidepressants, cocaine, or antipsychotics.
-
Patients with a history of seizures or epilepsy.
-
Individuals with head trauma or increased intracranial pressure.
Monitoring After Administration
Since flumazenil wears off quickly, patients must be monitored for re-sedation and respiratory depression for at least 2 hours after the last dose. Continuous monitoring of vital signs, oxygen saturation, and mental status is standard.
Importance in Emergency Medicine
Flumazenil has a controversial but vital role in emergency care. While it can be life-saving in acute benzodiazepine toxicity, its risks limit its widespread use. Many emergency physicians reserve it for very specific cases, such as:
Iatrogenic overdose – where too much benzodiazepine was given during a procedure.
Accidental ingestion in benzodiazepine-naïve individuals (e.g., children).
In most other overdose situations, supportive care (airway protection, IV fluids, and monitoring) is preferred.
Role in Anesthesia and Critical Care
Anesthesiologists often use benzodiazepines like midazolam for procedural sedation. At the end of surgery or diagnostic procedures, flumazenil allows rapid recovery so patients can awaken faster, reducing recovery room time.
In intensive care units, where patients may require sedation for ventilator support, flumazenil provides a safe option for reversing benzodiazepine effects when it is time to wean or assess neurologic function.
Coding and Documentation: Flumazenil in ICD-10
While flumazenil itself is a medication, documentation often involves coding for benzodiazepine overdose, poisoning, or adverse effects. Some relevant ICD-10 codes include:
T42.4X1A – Poisoning by benzodiazepines, accidental (initial encounter)
T42.4X2A – Intentional self-harm by benzodiazepines (initial encounter)
T42.4X3A – Assault involving benzodiazepines (initial encounter)
T42.4X4A – Benzodiazepine poisoning, undetermined intent (initial encounter)
Y45.0 – Adverse effects of benzodiazepines in therapeutic use
Flumazenil is not coded directly but is documented as part of the treatment plan. Accurate ICD-10 coding ensures insurance coverage and proper reporting of benzodiazepine-related cases.
Key Takeaways
-
Flumazenil is a benzodiazepine antagonist used primarily to reverse sedation or treat overdoses.
-
It acts quickly but has a short half-life, requiring close patient monitoring.
-
Though effective, its use is limited due to risks like seizures and withdrawal.
-
It is most beneficial in controlled environments such as hospitals, operating rooms, and intensive care units.
-
Accurate documentation and ICD-10 coding for benzodiazepine-related conditions are essential when flumazenil is used in treatment.
Conclusion
Flumazenil is a highly specialized medication that demonstrates how precise pharmacology can be both life-saving and risky. Its ability to reverse benzodiazepine sedation makes it invaluable in anesthesiology and emergency medicine. However, because of its potential to trigger seizures and withdrawal, its use must be cautious and carefully supervised.
Ultimately, flumazenil serves as a reminder that antidotes in medicine require as much respect and precision as the drugs they counteract. In the right hands and in the right setting, flumazenil remains a vital tool in modern healthcare.





Leave a Comment